History And Physical Examination Template
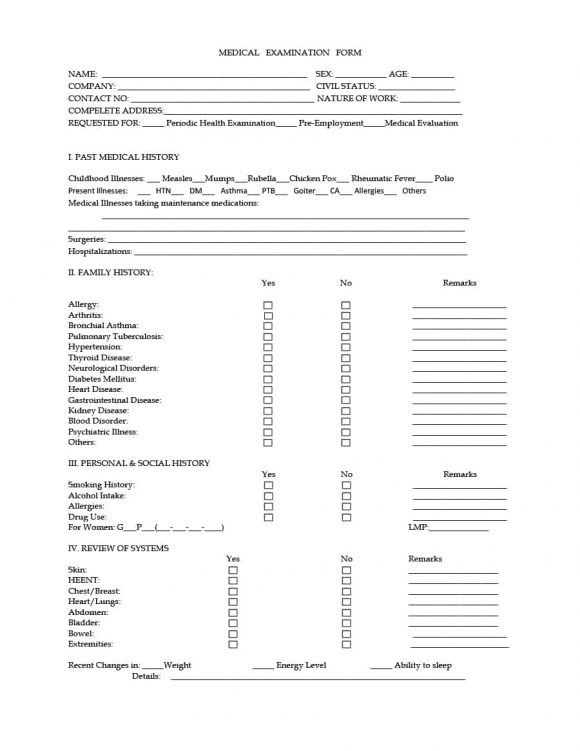
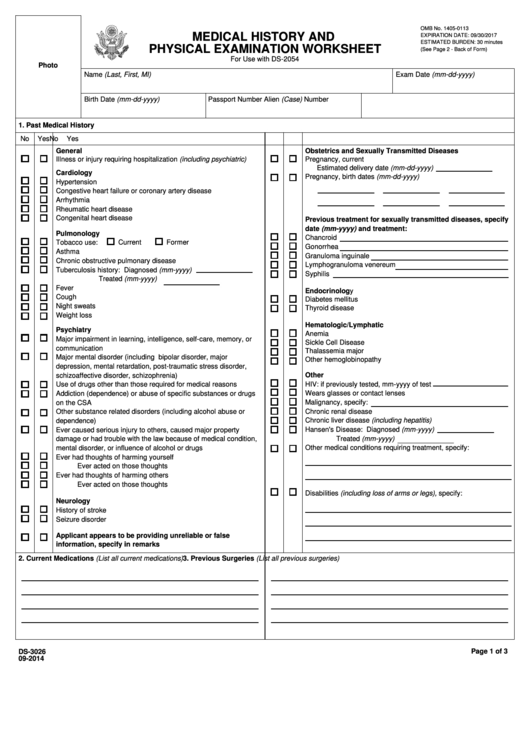
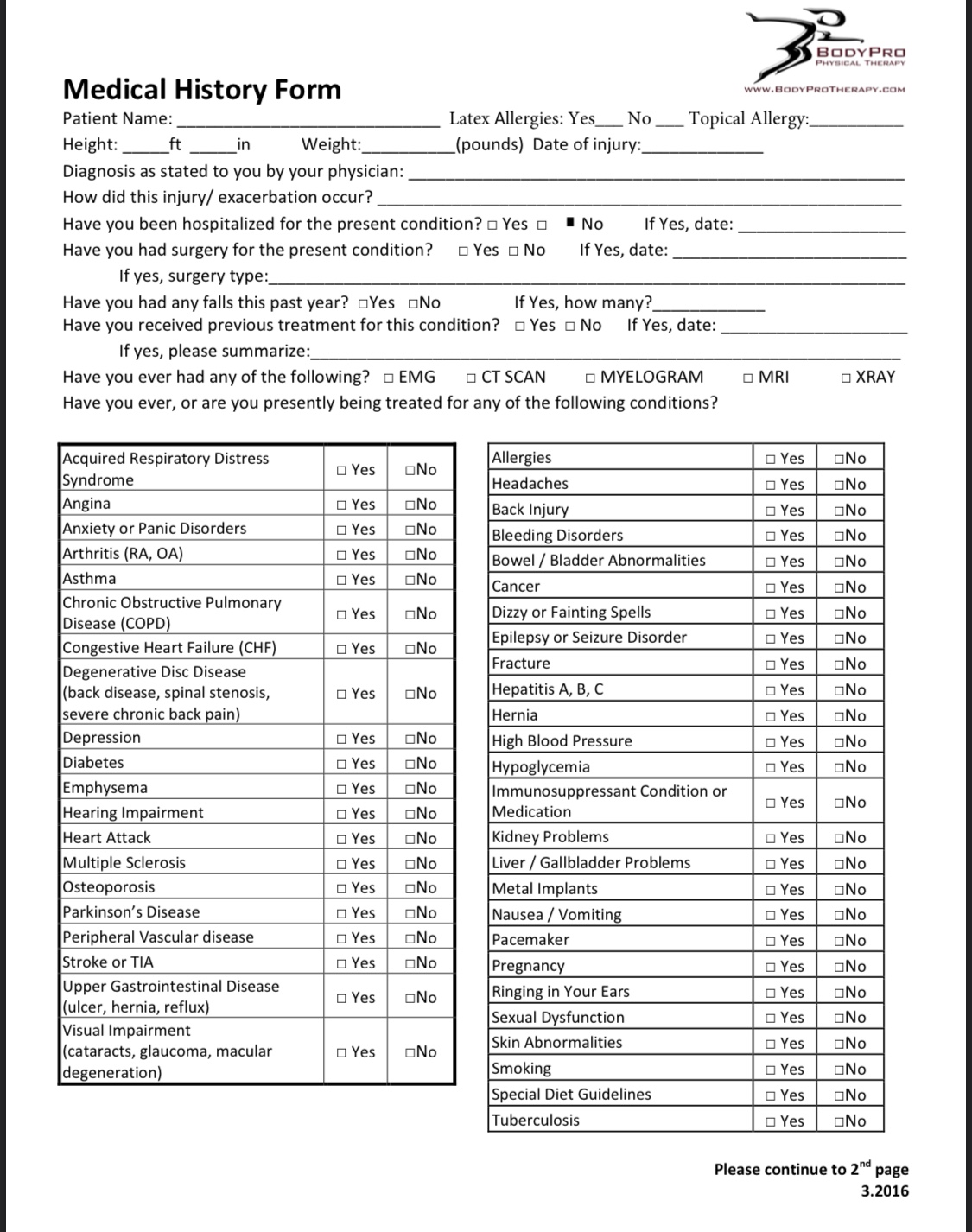
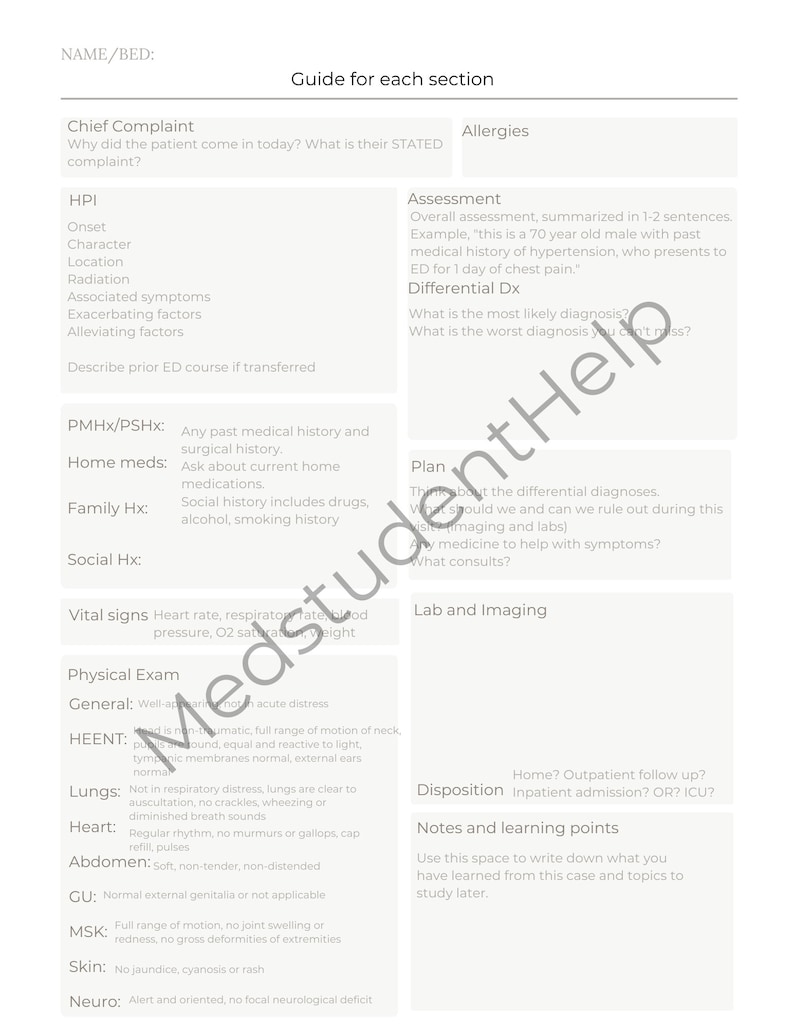
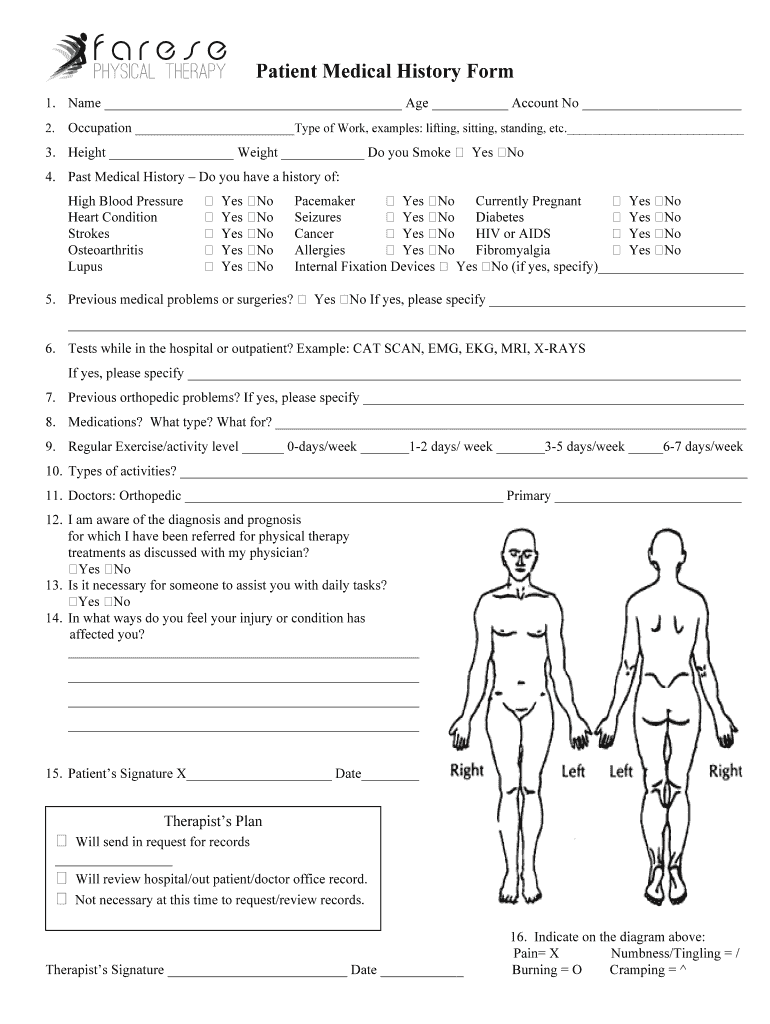
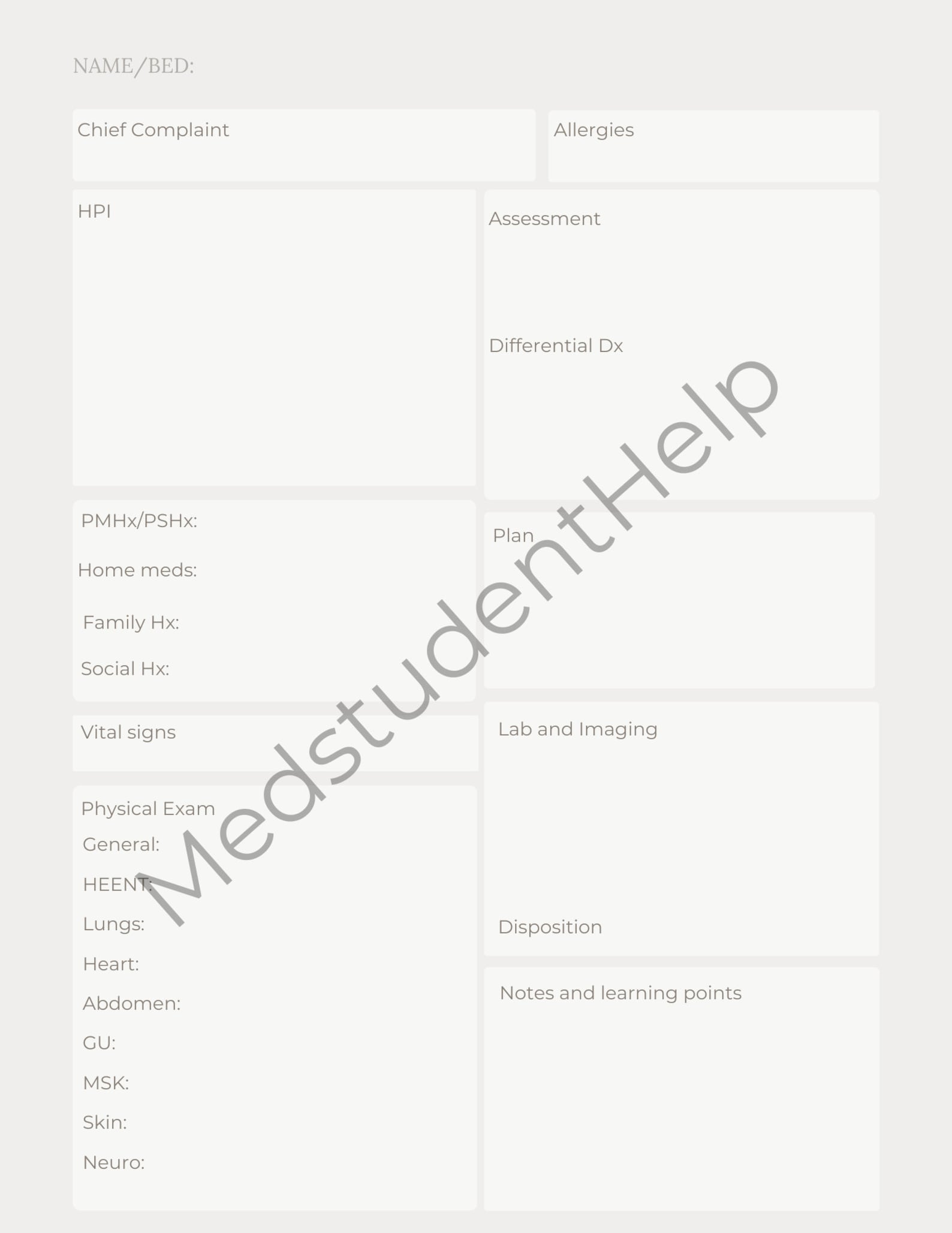
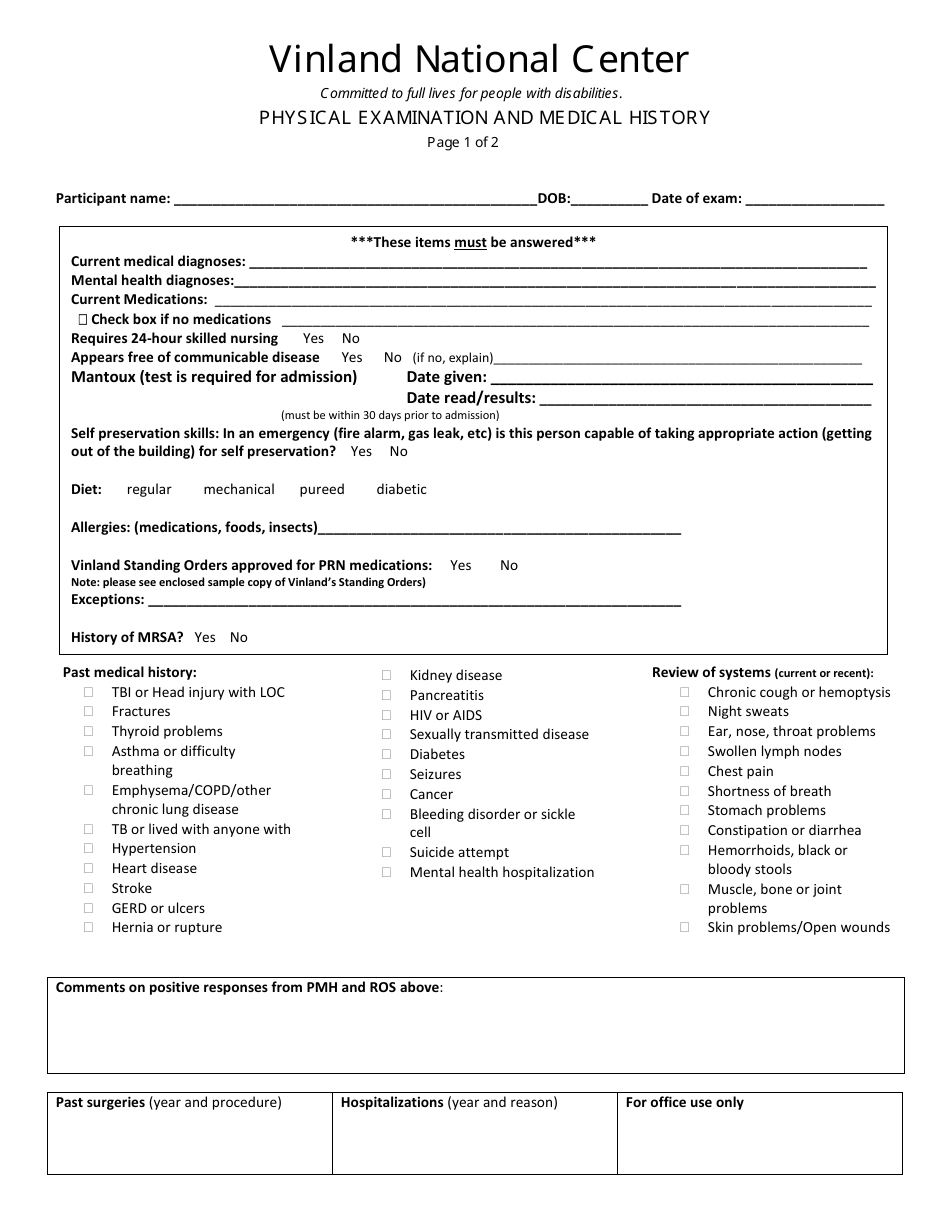
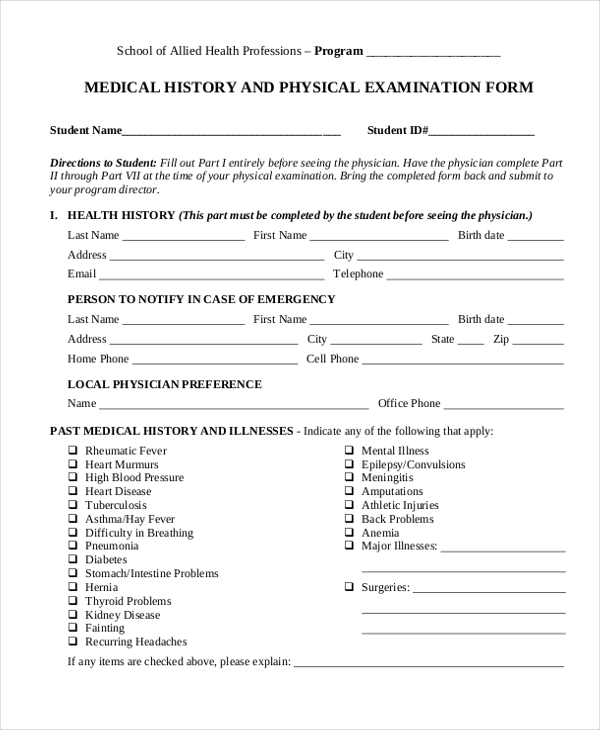
History And Physical Examination Template - This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. Upload this form to your american databank online account. In a focused history and physical, this exhaustive list needn’t be included. They can be used to collect important information. It includes sections for collecting the patient's identification data, chief complaints, history of present illness, past medical history, surgical history, family history, environmental history,. Initial clinical history and physical form author: strategies for efficient template utilization to maximize the benefits of using templates for physical therapy notes, consider the following suggestions: It is an important reference document that provides concise information about a patient's history and exam findings at the. This document provides a template for writing a history and physical examination report. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Clerks and residents on our surgical team are encouraged to use it or a similar system. This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. This simple template contains the headings for a classic history and physical examination report. This document provides templates for taking a. They can be used to collect important information. * required physical exam elements for h&p † required exam elements for all. Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes. She was first admitted to. It includes sections for collecting the patient's identification data, chief complaints, history of present illness, past medical history, surgical history, family history, environmental history,. Below is an example of thorough list. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. She was first admitted to. This simple template contains the headings for a. It is often helpful to use the. A simple online service to download legal templates and pdfs in minutes. Initial clinical history and physical form author: This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. A succinct description of the symptom (s) or. * required physical exam elements for h&p † required exam elements for all. History and physical template cc: This document provides a template for writing a history and physical examination report. Clerks and residents on our surgical team are encouraged to use it or a similar system. View, change, and fill in history and physical form quickly at formspal! It is often helpful to use the. U or iu, trailing zeros (1.0) or. It is an important reference document that provides concise information about a patient's history and exam findings at the. In a focused history and physical, this exhaustive list needn’t be included. History and physical template cc: The written history and physical (h&p) serves several purposes: This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. strategies for efficient template utilization to maximize the benefits of using templates for physical therapy notes, consider the following suggestions: A general physical exam template. Up to 40% cash back the document is an initial clinical history and physical form used to collect comprehensive patient information, including personal details, medical history, surgical. It is often helpful to use the. This simple template contains the headings for a classic history and physical examination report. A simple online service to download legal templates and pdfs in minutes.. A simple online service to download legal templates and pdfs in minutes. Initial clinical history and physical form author: View, change, and fill in history and physical form quickly at formspal! H&p templates are designed to guide healthcare professionals through the process of conducting a thorough patient examination, from the initial interview to the physical assessment. This document provides templates. * required physical exam elements for h&p † required exam elements for all. This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. In a focused history and physical, this exhaustive list needn’t be included. A succinct description of the symptom (s) or situation. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. It is an important reference document that provides concise information about a patient's history and exam findings at the. Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes. H&p templates are designed to guide healthcare professionals through the process. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. They can be used to collect important information. Past / family / social history (must include all 3) past medical / surgical hx/chronic medical. Upload this form to your american databank online account. This document contains a patient intake. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Up to 40% cash back the document is an initial clinical history and physical form used to collect comprehensive patient information, including personal details, medical history, surgical. The health history form is an important document used in medical settings to collect information about a patient’s health background. strategies for efficient template utilization to maximize the benefits of using templates for physical therapy notes, consider the following suggestions: It outlines the key sections to include such as the chief complaint, history of present illness,. Initial clinical history and physical form author: Clerks and residents on our surgical team are encouraged to use it or a similar system. View, change, and fill in history and physical form quickly at formspal! In a focused history and physical, this exhaustive list needn’t be included. This document provides a template for writing a history and physical examination report. A succinct description of the symptom (s) or situation responsible for the patient's presentation for health care. Below is an example of thorough list. Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes. Past / family / social history (must include all 3) past medical / surgical hx/chronic medical. They can be used to collect important information. It is an important reference document that provides concise information about a patient's history and exam findings at the.Physician History And Physical Template Master of Documents
History & Physical Exam
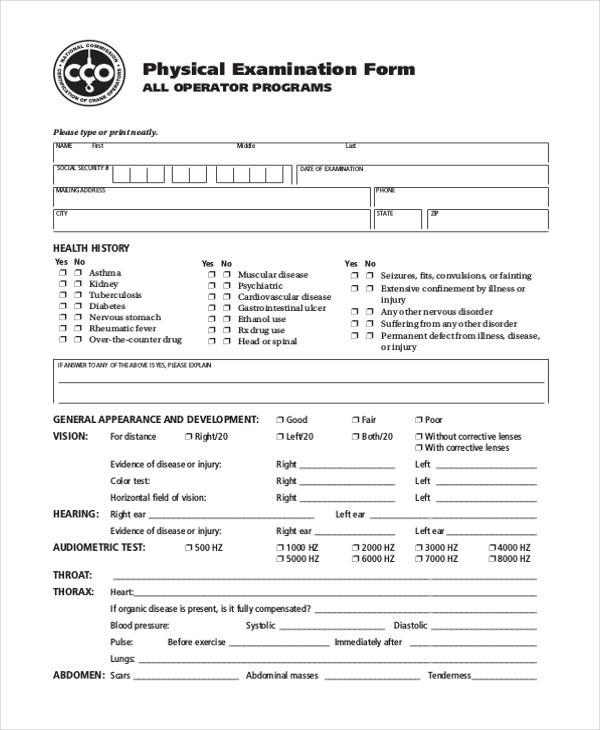
Fillable Ds3026 Form Medical History And Physical Examination
Comprehensive Health History Template
Printable History and Physical Exam Template Etsy
History And Physical Template
Printable History and Physical Exam Template Etsy
Physical Examination and Medical History Form Vinland National Center
History And Physical Template
Comprehensive Physical Exam Template Sample Templates
A Simple Online Service To Download Legal Templates And Pdfs In Minutes.
* Required Physical Exam Elements For H&P † Required Exam Elements For All.
Upload This Form To Your American Databank Online Account.
This Document Provides Templates For Taking A.
Related Post: