Progress Note Template Mental Health
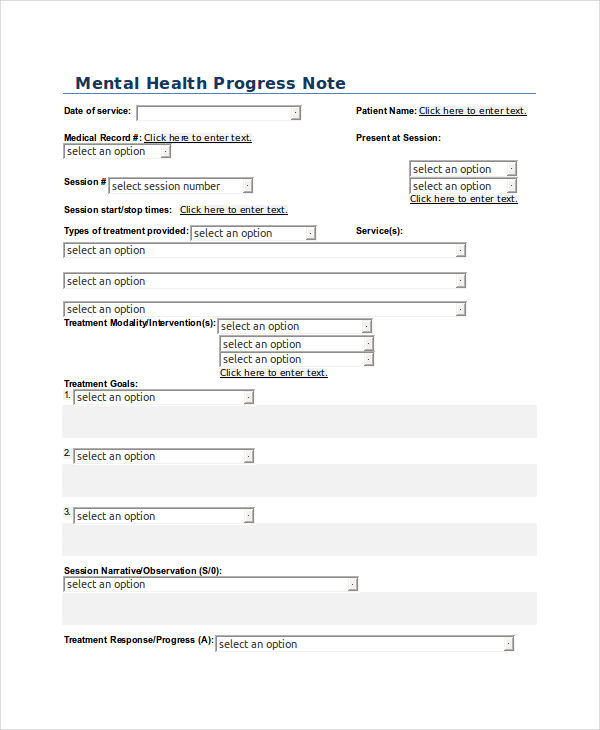
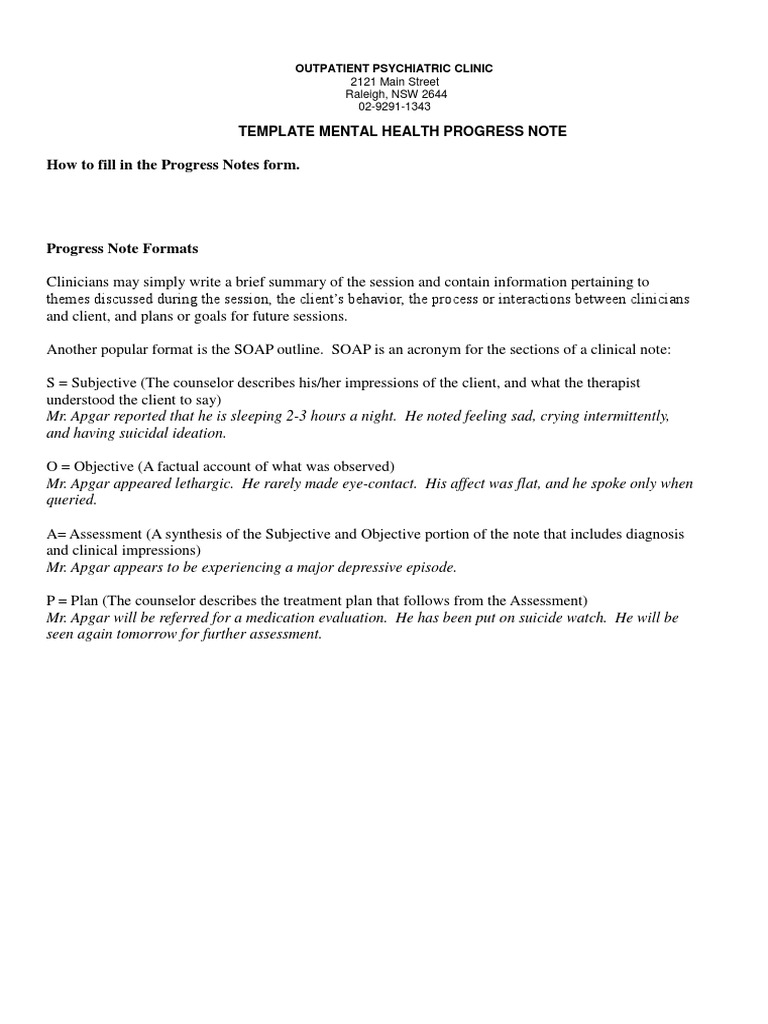
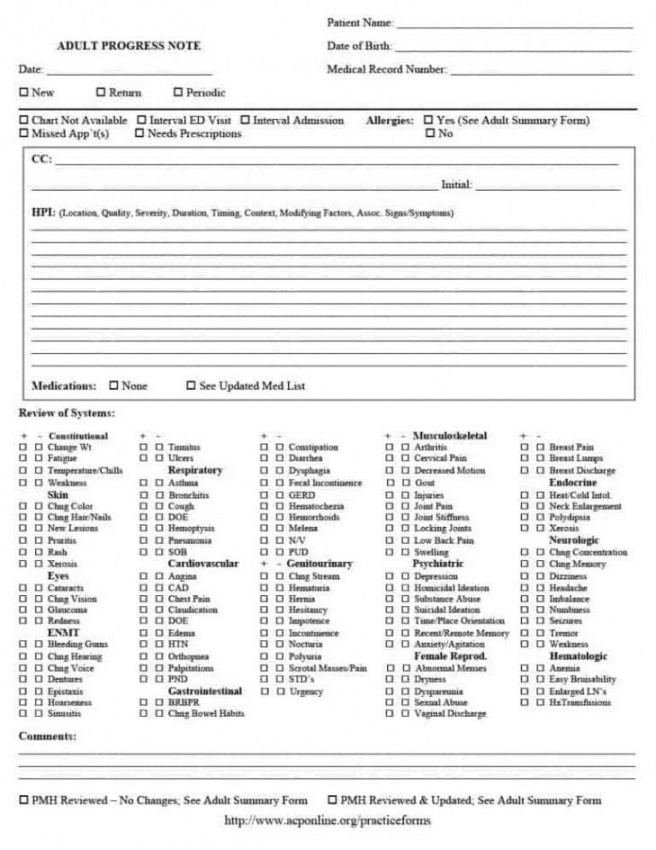
Progress Note Template Mental Health - Choosing the right template for mental health progress notes can significantly improve your clinical documentation process, enhance communication among healthcare professionals, and ultimately lead to better patient care. A progress note is an important part of a client’s mental health record, serving as a summary of the client’s status and progress in each psychotherapy session. They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences. They are commonly used by mental health professionals such as psychotherapists, psychiatrists, and other types of psychologists who want to ensure comprehensive coverage of patient care and treatment goals for people dealing with emotional. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. Soap notes are among the most commonly used progress note formats in healthcare settings, including mental health practices. Learn how to write progress notes mental health professionals can rely on, with actionable tips, detailed examples, and structured templates like soap, dap, and birp for streamlined documentation. Three of the most common progress note templates include: This structured approach helps therapists organize their thoughts, document relevant information, and communicate. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. Discover how to write perfect notes with different mental health progress note templates and examples designed for mental health professionals. Soap notes are among the most commonly used progress note formats in healthcare settings, including mental health practices. Explore expert mental health progress note templates & examples to enhance clinical documentation, streamline client care, and improve treatment outcomes. Learn how to write progress notes mental health professionals can rely on, with actionable tips, detailed examples, and structured templates like soap, dap, and birp for streamlined documentation. This format allows the provider to document their observations of the client and the session, and how they’re approaching the care plan. A progress note is an important part of a client’s mental health record, serving as a summary of the client’s status and progress in each psychotherapy session. Using structured templates like soap, dap, and birp formats can save time, improve accuracy, and enhance collaboration between providers. Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. Soap notes are among the most commonly used progress note formats in healthcare settings, including mental health practices. Using structured templates like soap, dap, and birp formats can save time, improve accuracy, and enhance collaboration between providers. Learn how to write progress notes mental health professionals can rely on, with actionable tips, detailed examples, and structured templates like soap, dap,. Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. Three of the most common progress note templates include: This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. This structured approach helps therapists organize their thoughts, document relevant information, and communicate. They’re instrumental in monitoring a patient’s. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences. This structured approach helps therapists organize their thoughts, document relevant information, and communicate. Discover how to write perfect notes with different mental. This format allows the provider to document their observations of the client and the session, and how they’re approaching the care plan. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. They are commonly used by mental health professionals such as psychotherapists, psychiatrists, and other types of psychologists who want to. This format allows the provider to document their observations of the client and the session, and how they’re approaching the care plan. Most therapists and mental health professionals use a progress note template to help with documentation. Discover how to write perfect notes with different mental health progress note templates and examples designed for mental health professionals. A progress note. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. This structured approach helps therapists organize their thoughts, document relevant information, and communicate. Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. Learn how to write progress notes mental health professionals can rely on, with actionable tips,. Three of the most common progress note templates include: Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. Soap notes are among the most commonly used progress note formats in healthcare settings, including mental health practices. They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. Learn how to write progress notes mental health professionals can rely on, with actionable tips, detailed examples, and structured templates like soap, dap, and birp for streamlined documentation. A progress note is an important part of a client’s mental health record, serving. Most therapists and mental health professionals use a progress note template to help with documentation. Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. This article highlights 18 effective templates tailored for various therapy settings, including individual, couples, group, and crisis intervention. Soap notes are among the most commonly used progress note formats in healthcare. Soap notes are among the most commonly used progress note formats in healthcare settings, including mental health practices. Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. This format allows the provider to document their observations of the client and the session, and how they’re approaching the care plan. A progress note is an important. Learn how to write progress notes mental health professionals can rely on, with actionable tips, detailed examples, and structured templates like soap, dap, and birp for streamlined documentation. Three of the most common progress note templates include: Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. This format allows the provider to document their observations of the client and the session, and how they’re approaching the care plan. They are commonly used by mental health professionals such as psychotherapists, psychiatrists, and other types of psychologists who want to ensure comprehensive coverage of patient care and treatment goals for people dealing with emotional. This structured approach helps therapists organize their thoughts, document relevant information, and communicate. Soap notes are among the most commonly used progress note formats in healthcare settings, including mental health practices. Choosing the right template for mental health progress notes can significantly improve your clinical documentation process, enhance communication among healthcare professionals, and ultimately lead to better patient care. Discover how to write perfect notes with different mental health progress note templates and examples designed for mental health professionals. Most therapists and mental health professionals use a progress note template to help with documentation. They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences.Mental Health Progress Note Template Free Printable Templates
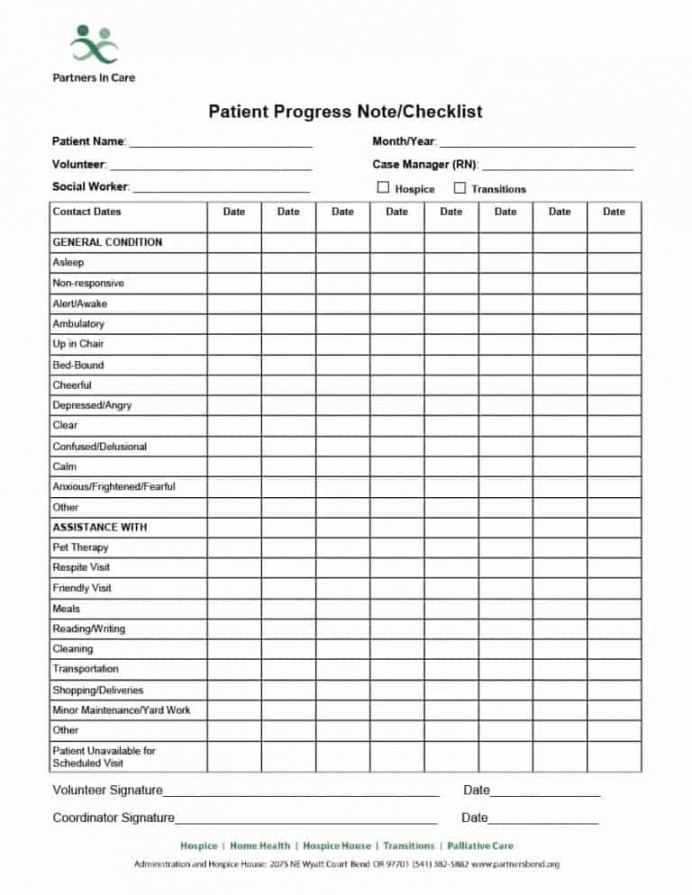
43 progress notes templates mental health psychotherapy nursing Artofit
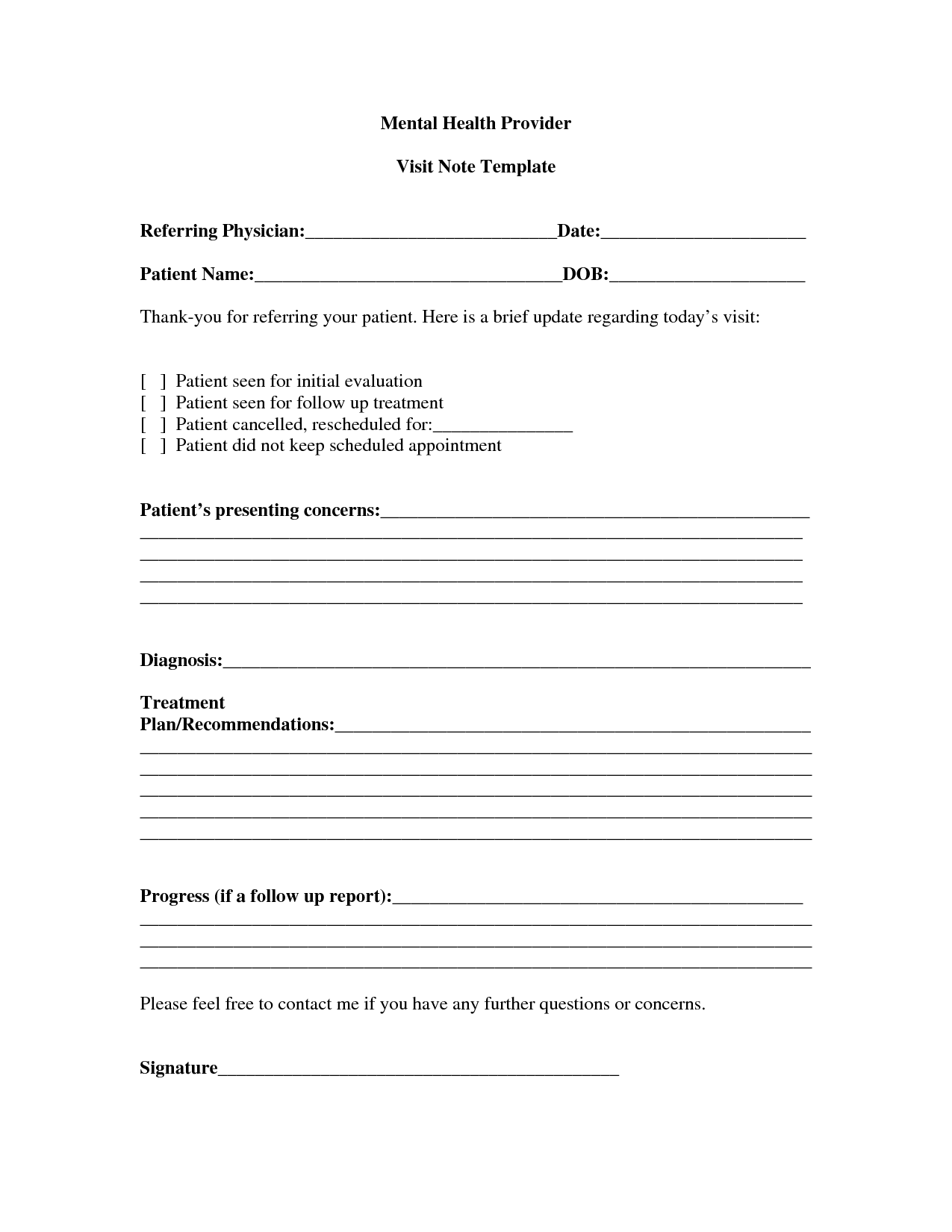
Mental Health Progress Note Template PARAHYENA
43 Progress Notes Templates [Mental Health Psychotherapy Psychiatry
Mental Health Progress Note Template PARAHYENA
Sample Mental Health Progress Note Anxiety Psychotherapy
Explore Our Sample Of Outpatient Psychiatric Progress Note Soap Note
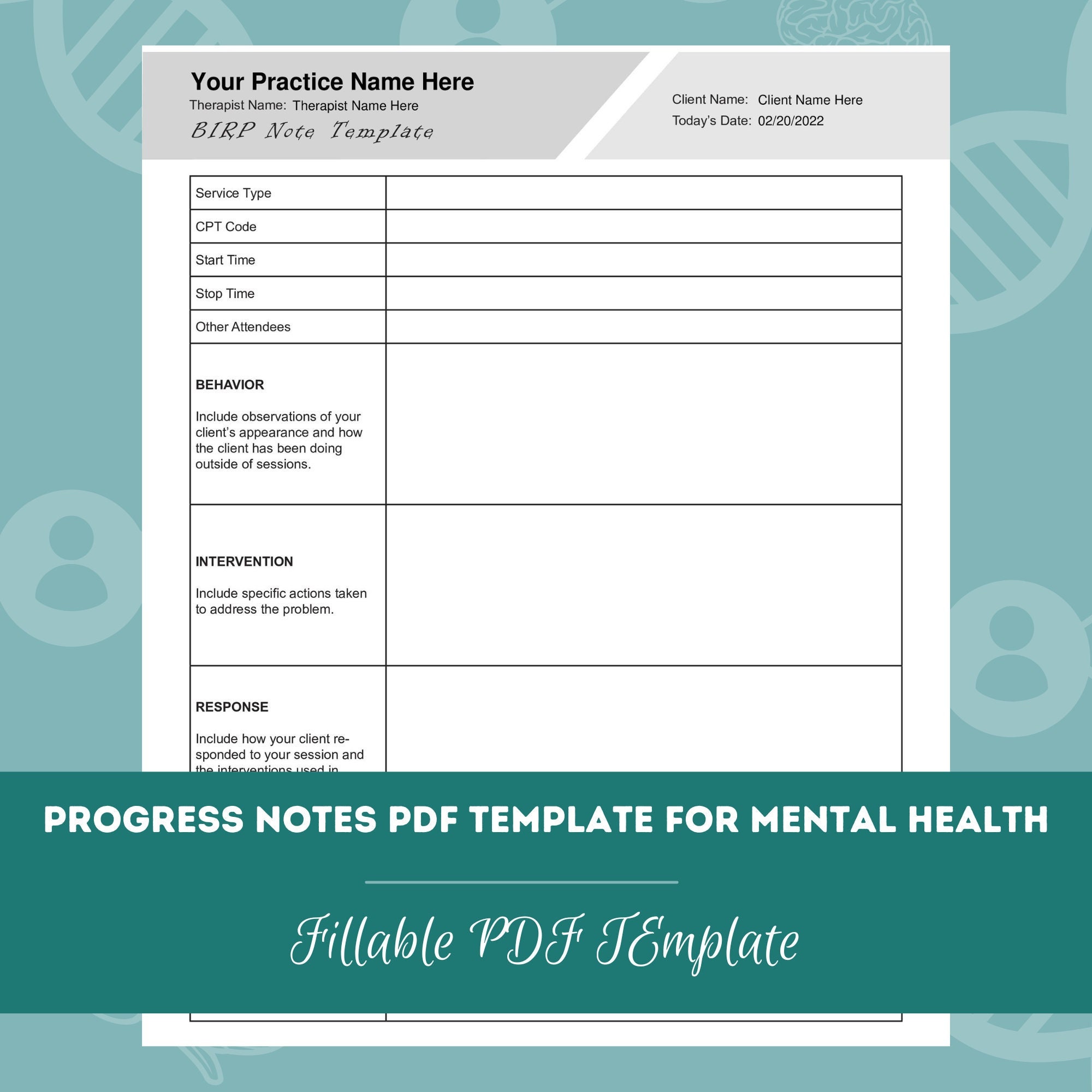
Progress Notes PDF Templates for Mental Health Editable / Fillable PDF
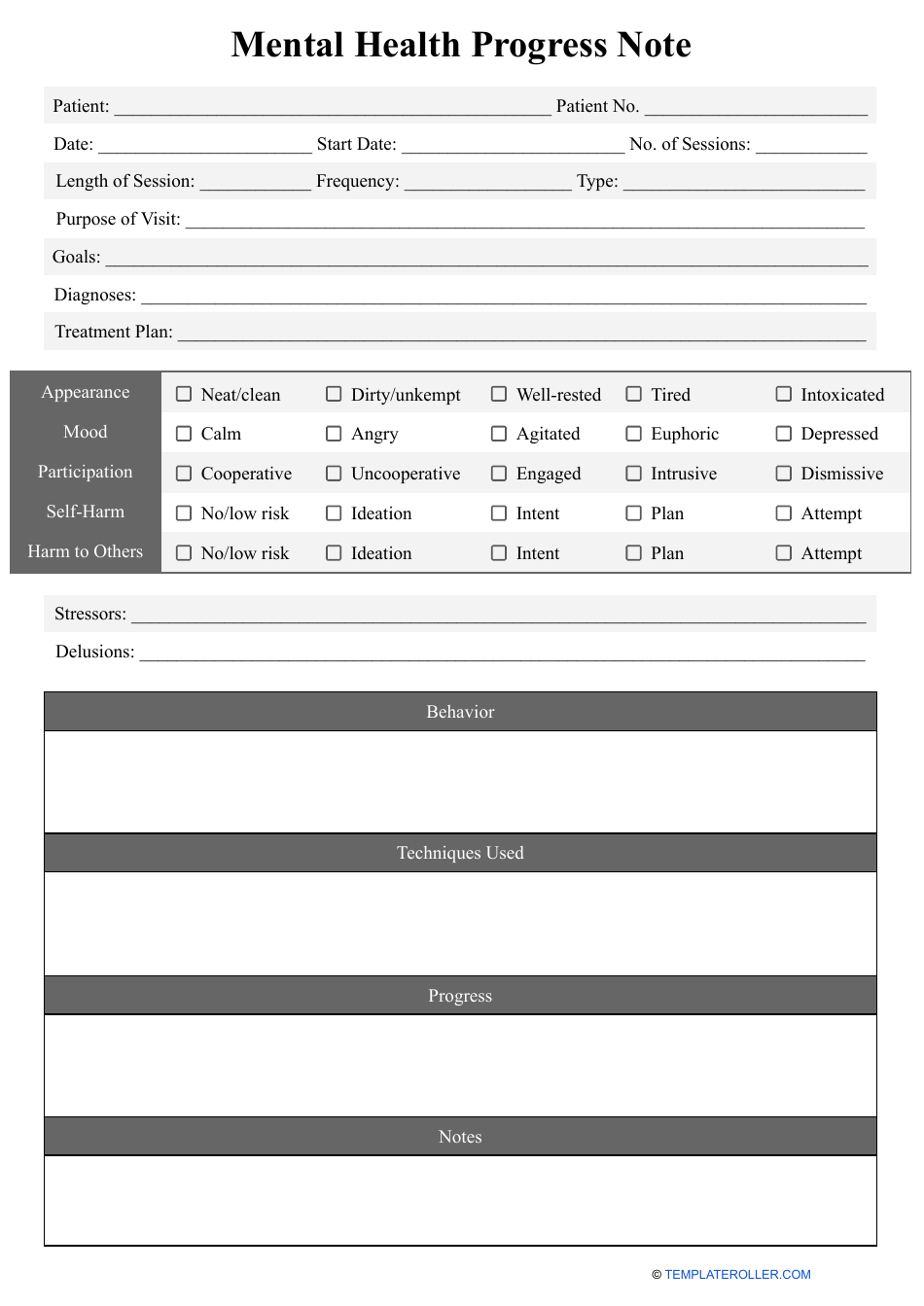
Mental Health Progress Note Template Download Printable PDF
Free Printable Mental Health Progress Notes Printable Templates
This Article Highlights 18 Effective Templates Tailored For Various Therapy Settings, Including Individual, Couples, Group, And Crisis Intervention.
Explore Expert Mental Health Progress Note Templates & Examples To Enhance Clinical Documentation, Streamline Client Care, And Improve Treatment Outcomes.
Using Structured Templates Like Soap, Dap, And Birp Formats Can Save Time, Improve Accuracy, And Enhance Collaboration Between Providers.
A Progress Note Is An Important Part Of A Client’s Mental Health Record, Serving As A Summary Of The Client’s Status And Progress In Each Psychotherapy Session.
Related Post: