Psych Soap Note Template
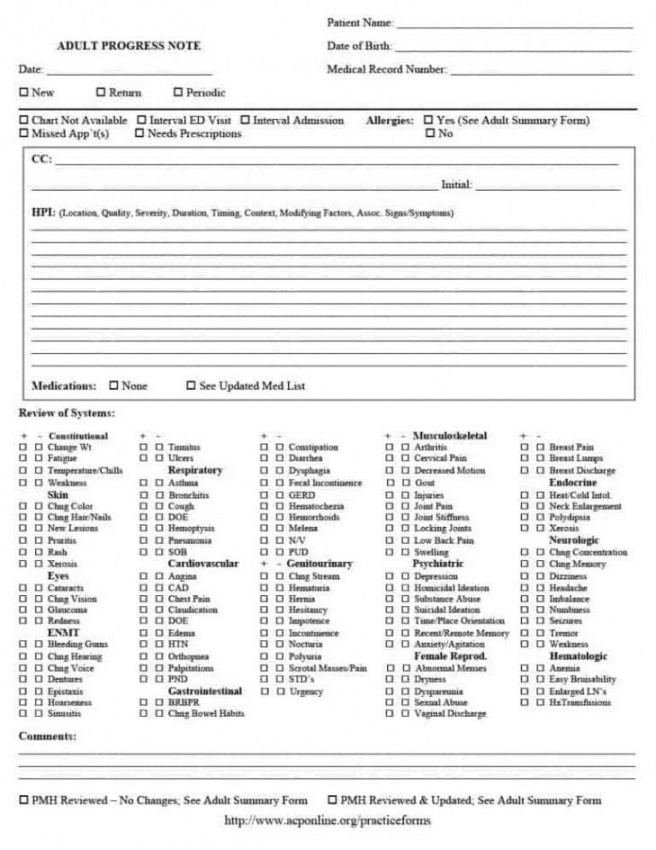
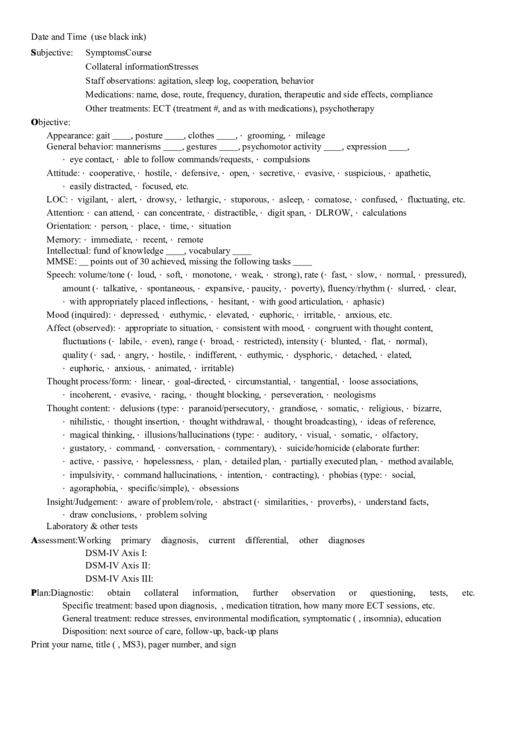
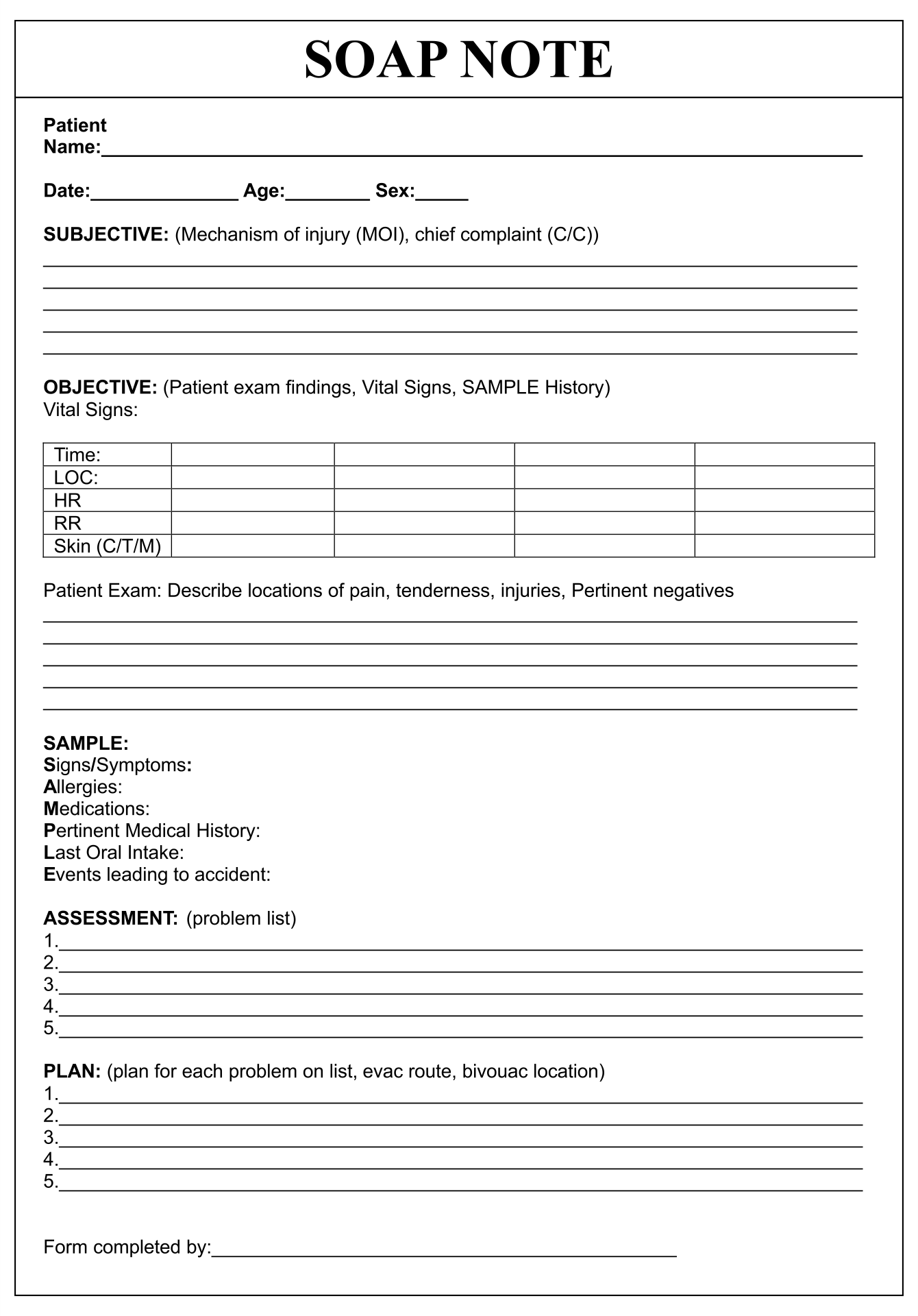
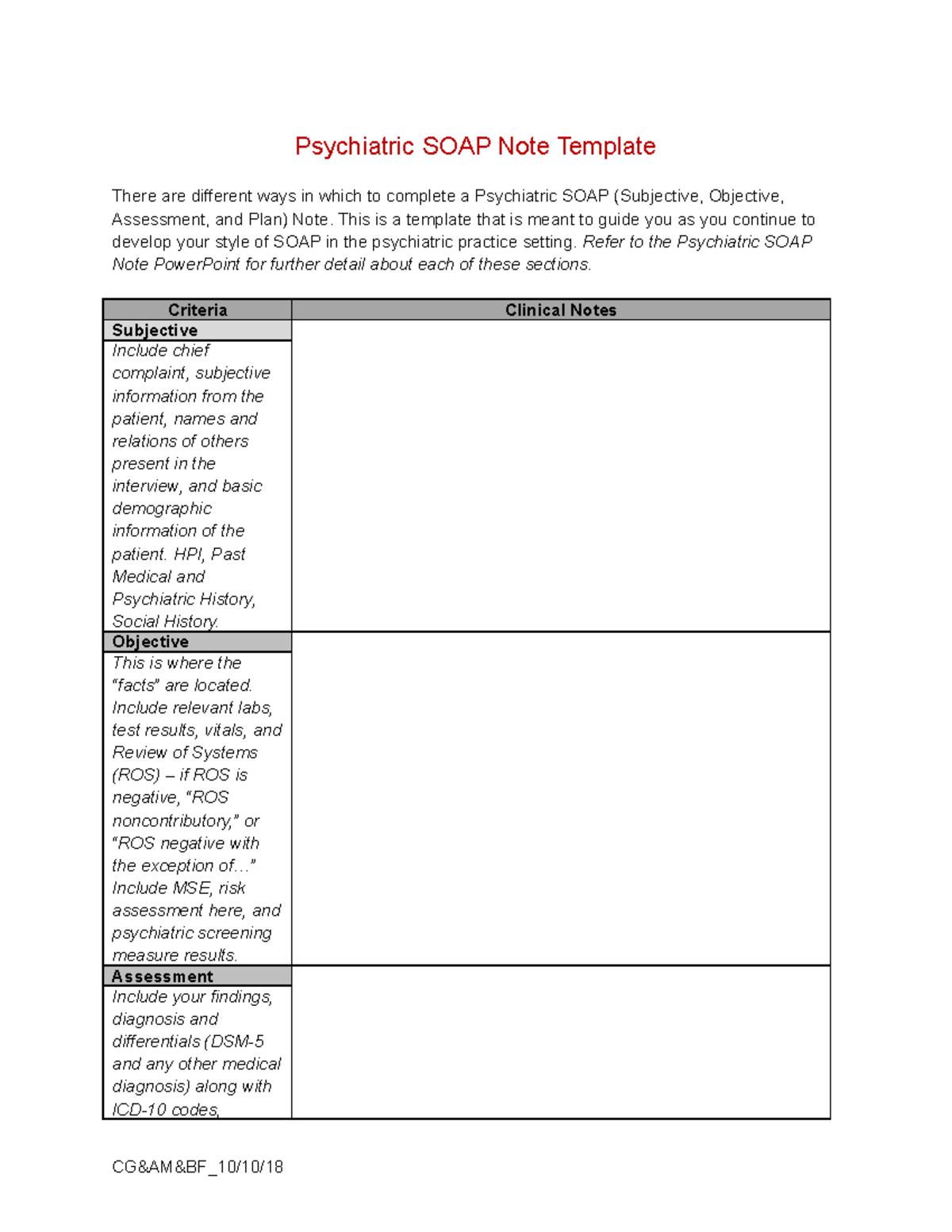
Psych Soap Note Template - The acronym, soap, stands for. This guide provides detailed instructions for each section of a soap note, helping you understand the. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. This is a template that is meant to. In this post, we will review what soap notes are, how to write a soap note, tips for. Learn what soap notes are, how to write them, and why they are important for counseling and mental health professionals. One of the most common and effective techniques to document a session is called writing soap notes. All other text was created by clicking templated content buttons. When you have these free editable samples, you. You'll also find sample soap notes, including counseling examples. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Using a soap note template can help you include all the essential elements of a soap note in a consistent way. Each example provides detailed insights into the subjective, objective, assessment, and plan components of soap notes, offering valuable templates for. Plus, templates can save you time and reduce the stress of trying to. Writing a mental health soap note (subjective, objective, assessment, and plan) is a common method behavioral healthcare professionals use to document patient encounters. Learn what soap notes are, how to write them, and why they are important for counseling and mental health professionals. This guide provides detailed instructions for each section of a soap note, helping you understand the. In psychology and psychiatry, writing soap notes must be clear and concise because it involves patients’ information which essential for his or her continuum of care. All other text was created by clicking templated content buttons. One of the most common and effective techniques to document a session is called writing soap notes. This is a template that is meant to. In psychology and psychiatry, writing soap notes must be clear and concise because it involves patients’ information which essential for his or her continuum of care. A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. This guide provides detailed instructions for each section of. The acronym, soap, stands for. Writing a mental health soap note (subjective, objective, assessment, and plan) is a common method behavioral healthcare professionals use to document patient encounters. Using a soap note template can help you include all the essential elements of a soap note in a consistent way. The only words typed are highlighted in yellow. One of the. Mental health providers will find soap notes beneficial for creating treatment plan documentation in particular. This sample inpatient psychiatric chart was created in icanotes. Each example provides detailed insights into the subjective, objective, assessment, and plan components of soap notes, offering valuable templates for. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). One of the most common and effective techniques to document a session is called writing soap notes. Soap notes can be used by many different providers across different medical. A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. Plus, templates can save you time and reduce the stress of trying to. In. Soap notes are essential for effective patient care and documentation in psychiatry. All other text was created by clicking templated content buttons. This guide provides detailed instructions for each section of a soap note, helping you understand the. Download free mental health soap note templates to take efficient notes during counseling and provide your patient with the best support possible.. When you have these free editable samples, you. In this article, we’ll show you how to write a soap note for mental health. Soap notes can be used by many different providers across different medical. A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. Soap note example and template for for psychiatrists. Plus, templates can save you time and reduce the stress of trying to. Integration with client records and appointment schedules. Soap notes can be used by many different providers across different medical. One of the most common and effective techniques to document a session is called writing soap notes. Soap note example and template for for psychiatrists. Download a free editable pdf template to organize your client. All other text was created by clicking templated content buttons. Soap notes can be used by many different providers across different medical. This guide provides detailed instructions for each section of a soap note, helping you understand the. In this article, we’ll show you how to write a soap note. All other text was created by clicking templated content buttons. The only words typed are highlighted in yellow. Soap notes can be used by many different providers across different medical. In psychology and psychiatry, writing soap notes must be clear and concise because it involves patients’ information which essential for his or her continuum of care. In this post, we. Soap notes are essential for effective patient care and documentation in psychiatry. The acronym, soap, stands for. In this article, we’ll show you how to write a soap note for mental health. This guide provides detailed instructions for each section of a soap note, helping you understand the. In psychology and psychiatry, writing soap notes must be clear and concise. A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. Soap notes are essential for effective patient care and documentation in psychiatry. Psychiatrist soap notes will primarily concentrate on the medical aspects of their treatment plan, such as the management of their. This is a template that is meant to. Soap note example and template for for psychiatrists. This sample inpatient psychiatric chart was created in icanotes. Download a free editable pdf template to organize your client. In this article, we have given some free psychiatric soap note samples for you which are available in microsoft word format. Mental health providers will find soap notes beneficial for creating treatment plan documentation in particular. The acronym, soap, stands for. When you have these free editable samples, you. Learn what soap notes are, how to write them, and why they are important for counseling and mental health professionals. Each example provides detailed insights into the subjective, objective, assessment, and plan components of soap notes, offering valuable templates for. In psychology and psychiatry, writing soap notes must be clear and concise because it involves patients’ information which essential for his or her continuum of care. Using a soap note template can help you include all the essential elements of a soap note in a consistent way. This guide provides detailed instructions for each section of a soap note, helping you understand the.Explore Our Sample Of Outpatient Psychiatric Progress Note Soap Note
SOAP Notes for Psychology Template & Example Free PDF Download
Soap Note Template 34 PDF Psychotherapy Mental Health
Psychiatry Progress Note Template & Example Free PDF Download
S.o.a.p. Note Template For Psychiatry printable pdf download
Counseling Soap Note Templates 10 Free PDF Printables Printablee
Soap Notes Mental Health Template PARAHYENA
Sample Psychiatric Soap Note
7+ FREE Psychiatric SOAP Note Samples in MS WORD Templates Show
6+ Soap Note Templates Free Word Documents Download Free & Premium
Soap Notes Can Be Used By Many Different Providers Across Different Medical.
One Of The Most Common And Effective Techniques To Document A Session Is Called Writing Soap Notes.
In This Article, We’ll Show You How To Write A Soap Note For Mental Health.
The Only Words Typed Are Highlighted In Yellow.
Related Post: